IMPLANT DENTISTRY
DENTAL CROWNS
DENTAL BRIDGES
Root Canal
SMILE AESTHETICS
Dental Veneers


Your gums shouldn’t bleed when you brush, but for millions of adults, they do. That’s not just bad luck; it’s the first sign of gum disease
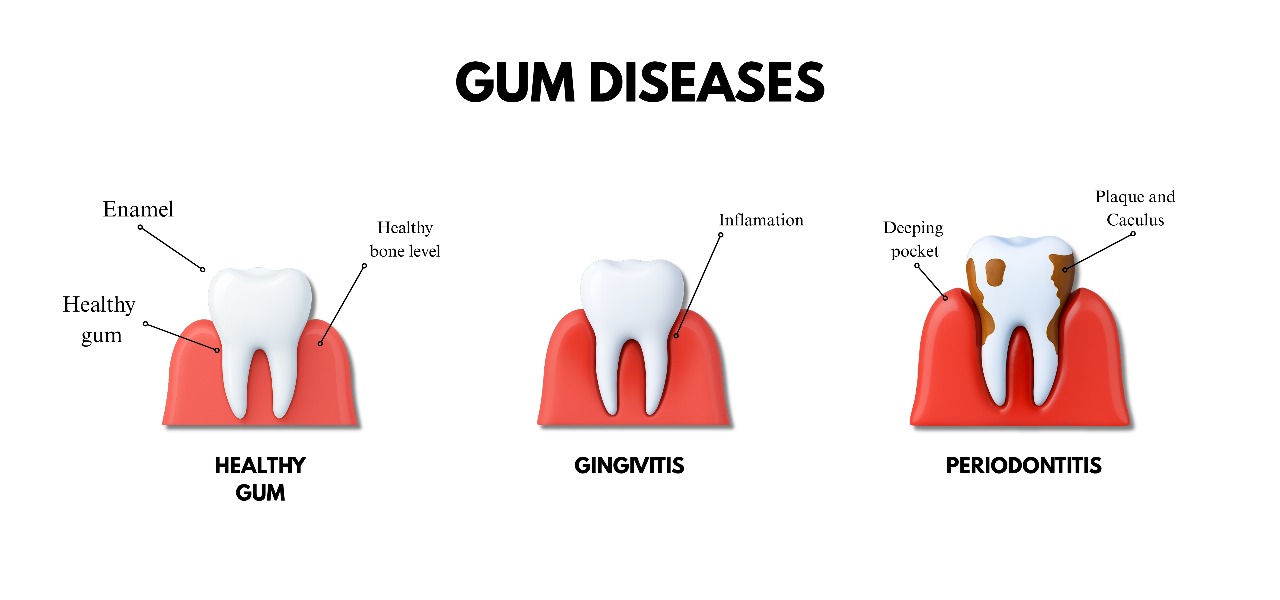
Gum disease is a bacterial infection of the gums and the supporting tissues around the teeth. This disease can develop into Gingivitis and periodontitis. So what is Gingivitis and Periodontitis?
In this article we’ll expand on how gum disease starts, what puts you at risk, and the stages and grades dentists use to describe the severity. We’ll also go through treatment options and how to prevent their progression.
Gum disease is a bacterial infection of the gums and the supporting tissue surrounding the teeth. It develops due to poor oral hygiene, diet, smoking, or certain health conditions.
Normally, you can eat and drink whatever you like without getting gum disease, but if you do without taking oral hygiene into account, then you’ll start developing gingivitis on your teeth.
Signs of gum disease and weakness;
Gum diseases are also known as gingivitis, as it is a form of gum disease that affects your teeth, and potentially could have an impact on your overall health.

This is the earliest stage of gum infection. It is caused by plaque buildup on the gum line.
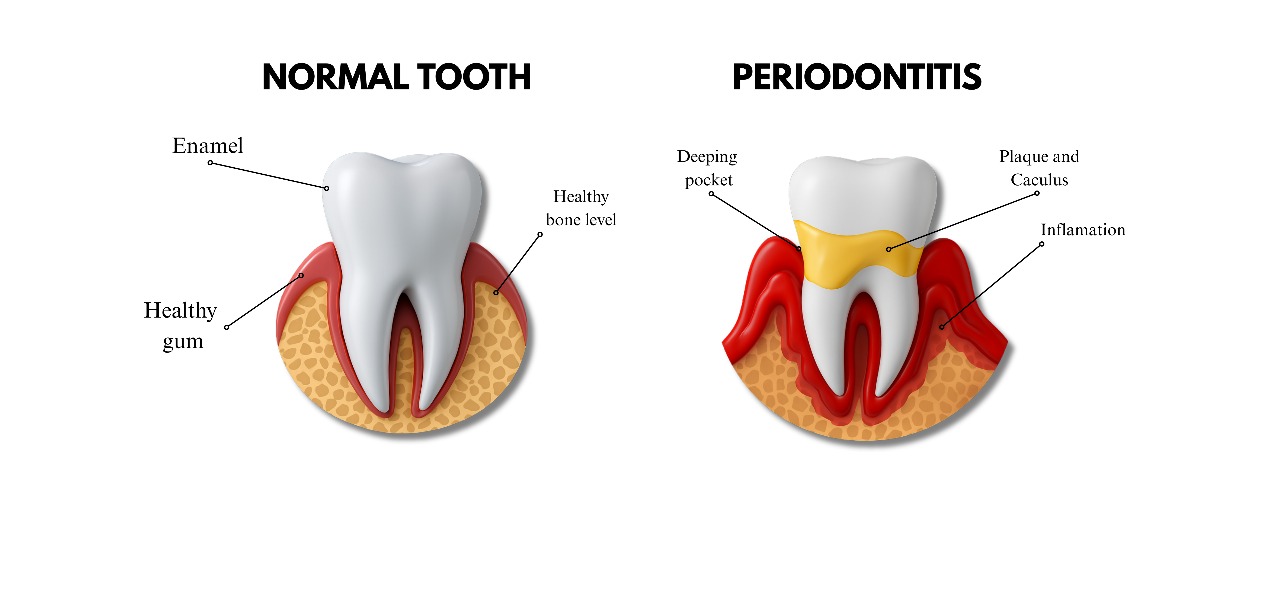
If you look at the picture on the left hand side, you’ll notice that the gum is equally colored. while the picture on the right hand side, you’ll notice that the gums are swollen and irritated.
Gingivitis is the earliest stage of developing periodontal disease, and the pathway is;
You have to be aware that there are two types of gingivitis; Plaque Induced, and Non-Plaque induced. We will explain each thoroughly, and tell you how to treat each in-your home’s comfort.
But, before we do that we have to tell you what are the symptoms of gingivitis;
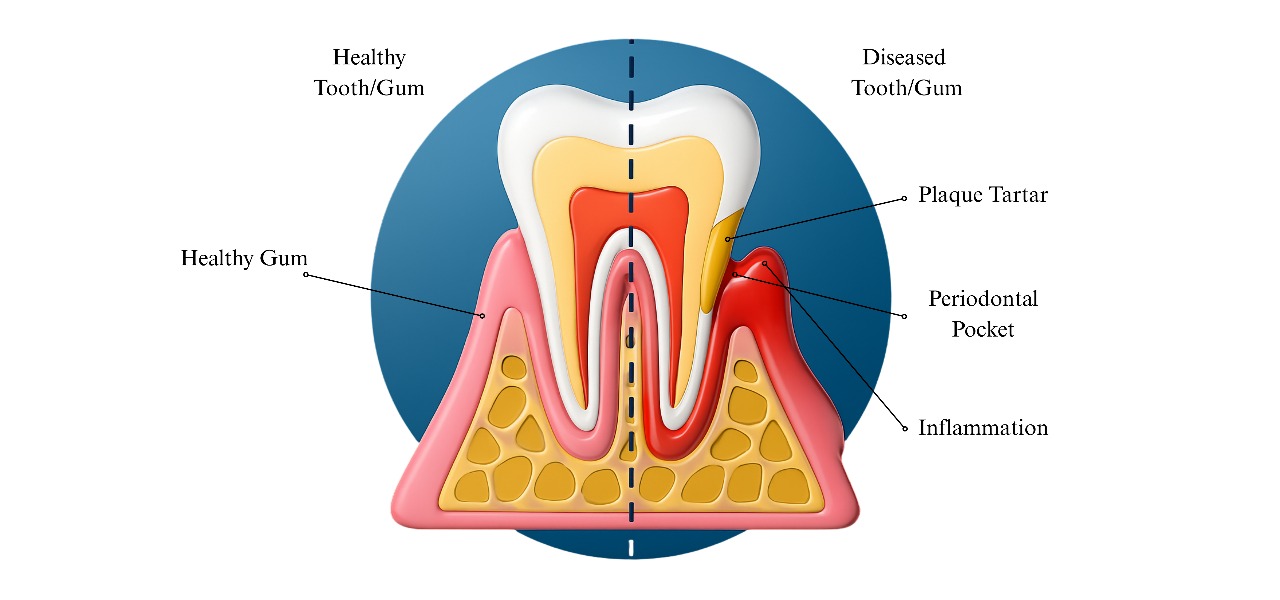
If your gum is that severely pressured by the plaque and tartar, it’s only natural to develop gum inflammation, which is your body’s natural response to fight off infections.
Next, let’s break down the stages, from reversible gingivitis to severe periodontitis
Gingivitis is a stage of gum disease that is reversible easily without doctor’s intervention. You would just need to change your habits, diet and plan more around what is healthy for you. Gingivitis is the early form of periodontitis.
On the other hand, Periodontitis is a severe gum infection that is the advanced stage of gum disease. It damages the soft tissue and, if left untreated, can destroy the bone that supports your teeth, leading to tooth loss.
Periodontitis is very dangerous if left untreated as its damage is often irreversible. It is important to know that there are four Gingivitis stages, and three stages of progression; slow,moderate and rapid. Tooth loss will depend on your state of progression.
While in this stage, there shouldn’t be pain, rather irritation. The next stage is definitely going to cause some discomfort.
Advanced symptoms are when gingivitis starts developing from plaque to tartar and inflames your gums. At this stage the damage starts to get irreversible, depending on how deep it reaches the support bones in your jaw.
These symptoms can range from;
While gum diseases rarely kill anyone in this stage, but if left untreated. It could contribute to life-threatening conditions like heart disease, or sepsis.
These signs are our indicators to pay attention to our dental health, and if you refusal to pay attention, you’ll go from mild gingivitis to tooth loss (periodontitis) in no time.
iStages & Grades of Progression
Stages of Periodontitis
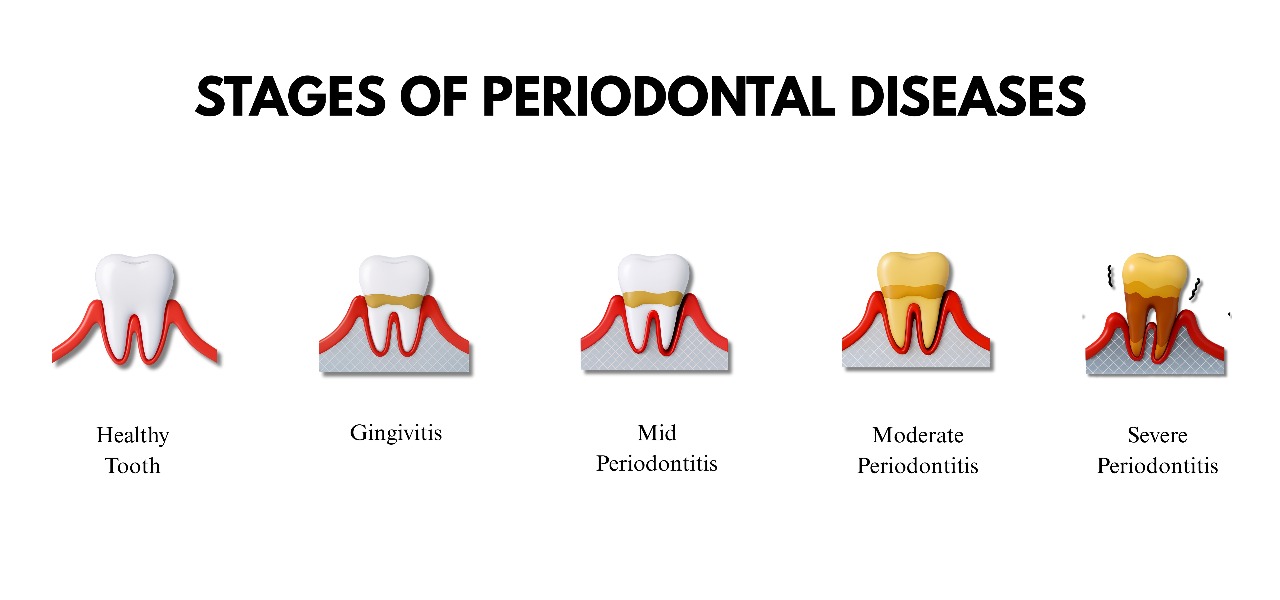
Gingivitis is the early stage, where inflammation is mild and is confined to the gums.
These are the defining elements that you have gingivitis;Plaque Buildup: The primary cause is the bacterial plaque at the gum line. This sticky film irritates the gum tissue.
Inflammation: The gums become inflamed in response to the bacteria. This is your body’s initial defense mechanism.
Bleeding: A key sign of gingivitis is that the gums bleed easily, often when you clean or floss your teeth.
No Bone or Tissue Loss: At this stage, the inflammation has not yet spread to the underlying bone or connective tissue that supports the teeth. This is a crucial distinction from more advanced stages.
Reversibility: Easy.
Stage 2 Early Periodontitis.
This is where it develops from gingivitis towards a full on Periodontitis
Deeper Pockets: The pockets between the teeth and gums are now deeper than in gingivitis (typically 3-4 millimeters).
Bone Loss: This is a key characteristic of periodontitis. The infection begins to destroy the underlying alveolar bone that holds the teeth in place. The bone loss at this stage is usually mild.
Receding Gums: The gums may visibly pull away from the teeth, making the teeth appear longer.
Slight Tooth Mobility: You may notice that one or more teeth feel slightly loose or are tender when you bite down.
Mouth odour: The bacteria in the periodontal pockets produce a foul odor, leading to persistent bad breath.
Reversibility: Possible
During this stage, professional dental treatment is crucial to halt the disease’s progression and prevent tooth loss
Increased Bone Loss: The biggest feature of this stage is moderate to severe bone loss, It is clearly visible on dental X-rays.
Deeper Pockets: The periodontal pockets have deepened to a range of 5–7 millimeters or more. These deep pockets are difficult to clean with routine cleaning and flossing, allowing bacteria to thrive.
Tooth Mobility: Due to the loss of bone and tissue support, the affected teeth may become noticeably loose or wobbly.
Further Gum Recession: The gums may continue to pull away from the teeth, exposing more of the tooth root and making teeth appear even longer.
Reversibility: Hard
During this stage, the first stages are enhanced, and more visible and painful.

This is the point of advanced periodontal disease where the damage is often irreversible, and requires immediate dental interference. Its defining features; are severe bone loss, and significant tooth mobility.
Severe Bone Loss: There is significant and often widespread bone loss, typically more than 50% of the tooth’s root length.
Deep Pockets: The periodontal pockets are very deep, usually 7 millimeters or more. These pockets are chronic reservoirs for bacteria that continue to destroy tissue and bone.
Significant Tooth Mobility and Shifting: The teeth are now very loose. They may have shifted out of their normal positions, creating gaps between them. Chewing is often very painful or impossible.
Likely Tooth Loss: At this stage, tooth loss is highly probable. The teeth may fall out on their own, or they may need to be extracted because they are no longer viable.
Reversibility: Very Difficult
Now that we’ve walked through the stages of gingivitis to advanced periodontitis, it is important to consider the rate of progression, which tells us how quickly the disease is moving.
There are three clinical grades of periodontal progression, Grade A (slow), Grade B (moderate), Grade C (rapid), and Grade D (Irreversible). These grades reflect how quickly disease advances and which risk factors are present.
In an study, this grading framework was formalized in 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions.
We’ll explore these stages, and break down the terminology in simpler terms.
| Grade | Description | Why it Progresses This Way | Typical Indicators | Risk Factors |
| Grade A (Slow) | Minimal bone or tissue loss over time. Stable, may not worsen quickly. | Patients usually have good oral hygiene, don’t smoke, and have well-controlled health. | Minimal bone loss relative to age. | None or very few healthy habits keep damage limited. |
| Grade B (Moderate) | Steady, measurable rate of bone loss that matches plaque levels. | Risks present such as inconsistent hygiene, smoking history, or diabetes. | Noticeable bone loss relative to age. | Light smoking, diabetes, poor diet, irregular dental care. |
| Grade C (Rapid) | Aggressive bone and tissue destruction; fastest progression. | Driven by strong risk modifiers like heavy smoking, uncontrolled diabetes, or genetics. | Early tooth mobility, severe bone loss for age. | Heavy smoking, poorly controlled diabetes, genetic predisposition. |
| Stage 4: Advanced Periodontitis | The most severe and destructive stage of gum disease. Immediate dental intervention is essential. | Severe gum recession, very loose or shifting teeth, painful chewing, deep pockets , pus or abscesses. | Extensive bone loss | Irreversible damage. Tooth loss is likely. Requires advanced dental treatment (scaling, surgery, or extraction). |
Understanding the grades of gum disease tells us how fast it can progress, but knowing isn’t enough. The real question is: what can you do to stop it?
We must begin, where the issue started, thus going back to ground zero. Gum diseases are what started it. Hence plaque removal is the single most important to prevent gum disease.
We’ve created a checklist to do at home to prevent plaque formation.

If you’re able, visit a dentist. As you must get a professional cleaning (prophylaxis) at-least every six months (More if your dentist recommends it). Two of the biggest modifiers that can affect your dental health are smoking, and poor blood sugar control. It is quite important to take care of your diet, and what goes in your body if you want to take care of your teeth.
A nutrient-rich diet and hydration support healing beyond what you think. Consuming vitamin C, and calcium rich foods goes a long way. These dietary measures are supportive, they could not replace scrubbing your teeth,flossing, or professional care.
If you’re looking for a solution for gingivitis in a week, there isn’t any. You have to be consistent with oral hygiene and what you consume. But on a positive note if you start implementing better diet and habits, you’ll lose it quickly with just that. Periodontitis can not be treated with at-home remedies alone, and it is a must to get professional help.
Gingivitis is a stage of gum disease that can develop into periodontitis, a serious dental threatening disease that can affect other bodily functions like the heart. You must be proactive with the treatments, and try to stop it as fast as you can early on. You must not hesitate to seek medical attention, if you’re feeling pain or sore gums.
Getting a dental visit once every 6 months is always encouraged and will act as a gum disease prevention.
If you’re looking for expert care, Dr. Cem Baysal has over 30 years of experience treating gum disease in Turkey.
Check the Turkeu teeth before and after